Physician’s Resources
Access the latest research and guidelines to practical tools and patient education materials tailored to support the diagnosis and management of breast density. Join our mission to improve patient outcomes by staying informed and equipped with Operation Breast Density.
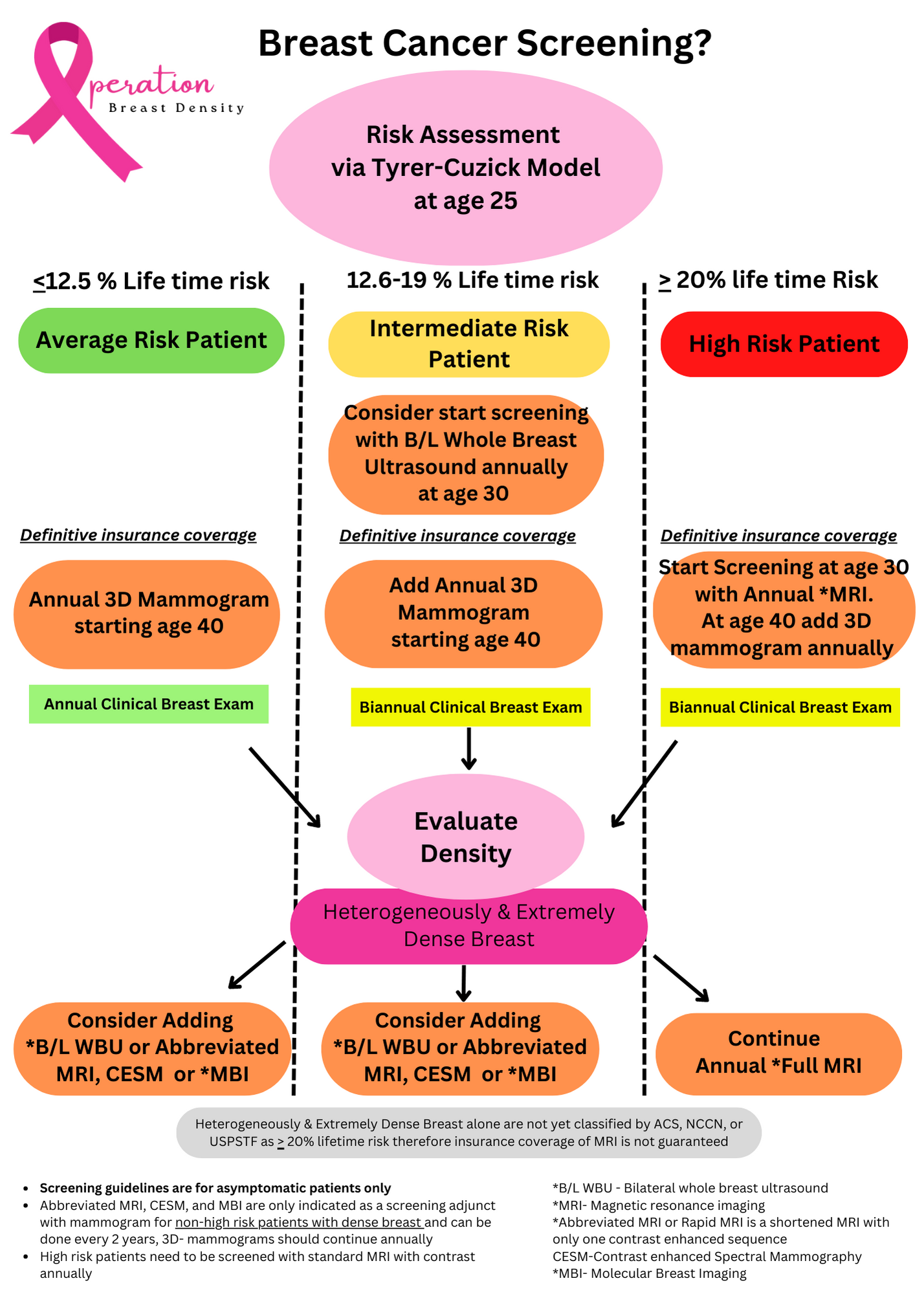
Breast Cancer Screening
Breast Cancer Screening should begin at age 25 with a calculation of the patients life time risk of breast cancer development.
A patient’s family history should be thoroughly evaluated to determine the need for genetic testing.
Average Risk Patients
A woman is considered to be at average risk if she doesn’t have a personal history of breast cancer, a strong family history of breast cancer, does NOT have Dense breasts, or does not have a genetic mutation known to increase risk of breast cancer and has not had chest radiation therapy before the age of 30.
A woman is considered an average risk therefore if her lifetime risk of breast cancer development is < 12.5%.
Recommendations are as follows:
Women at age 40 should start screening with a 3-D mammogram every year.
Low or Intermediate Patients and Patients with Dense Breasts
A woman is considered to be at intermediate risk if her lifetime risk of breast cancer development is 13-19 %.
Recommendations are as follows:
These women often need supplemental imaging annually in addition to 3-D Mammography to complete their breast cancer screening.
Supplemental imaging options are Whole Breast Ultrasounds, Contrast Enhanced Mammogram, Abbreviated/FAST MRI or MBI for Screening.
Discussion about what test is best should be done with the patients physician.
Risk stratifications of life time development of breast cancer calculated by the Tyrer-Cuzick Model can help guide decisions on supplemental imaging needed for these patients.
High risk women
A patient is considered high risk if her lifetime risk of breast cancer development is 20% or greater.
A patient is also considered high risk if she has one of the following: known BRCA1 or BRCA2 gene mutation (based on having had genetic testing, first-degree relative with a BRCA1 or BRCA2 gene mutation, and have not had genetic testing themselves, Had radiation therapy to the chest when they were between the ages of 10 and 30 years, Have Li-Fraumeni syndrome, Cowden syndrome, or Bannayan-Riley-Ruvalcaba syndrome, or have first-degree relatives with one of these syndromes
Recommendation is as followed:
at age 25 with biannual clinical breast exams.
at age 30, Full Breast MRI and a mammogram every year
Check out Our Annual Breast Cancer Symposium!
To learn more about screening a high-risk patient and a patient with dense breasts, be sure to attend our annual breast cancer symposium. Visit the upcoming events page for more information.
References
1. American Cancer Society Breast Cancer Screening Guidelines. https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html
2. NCCN Breast Cancer Screening guidelines. https://www.nccn.org/patientresources/patient-resources/guidelines-for-patients/guidelines-for-patients-details?patientGuidelineId=66
3. Comstock C, Gatsonis C, Newstead G et al. Comparison of Abbreviated Breast MRI vs Digital Breast Tomosynthesis for Breast Cancer Detection Among Women With Dense Breasts Undergoing Screening. JAMA. 2020;323(8):746-756. doi:10.1001/jama.2020.0572
4. Gao Y, Heller S et al. Abbreviated and Ultrafast Breast MRI in Clinical Practice. RadioGraphics 2020; 40:1507–1527. https://doi.org/10.1148/rg.2020200006
5. Brentnall A, Cuzick J et al. Long-term Accuracy of Breast Cancer Risk Assessment Combining Classic Risk Factors and Breast Density. JAMA Oncol. 2018;4(9):e180174. doi:10.1001/jamaoncol.2018.0174
6. Reboljl et al. Addition of ultrasound to mammography in the case of dense breast tissue: systematic review and meta-analysis. British Journal of Cancer (2018) 118:1559–1570; https://doi.org/10.1038/s41416-018-0080-3
7. Harada-Shoji N et al. Evaluation of Adjunctive Ultrasonography for Breast Cancer Detection Among Women Aged 40-49 Years With Varying Breast Density Undergoing Screening Mammography A Secondary Analysis of a Randomized Clinical Trial. Oncology. 2021. JAMA Network Open. 2021;4(8):e2121505. doi:10.1001/jamanetworkopen.2021.21505
8. Monticciolo D et al. Breast Cancer Screening in Women at Higher-Than-Average Risk: Recommendations From the American College of Radiology. Journal of American College of Radiology. 2018;15:408-414.
9. Buchbergera W et al. Combined screening with mammography and ultrasound in a population based screening program. European Journal of Radiology. 2018. (101)24–29
10. Ritse M. Mann. Breast cancer screening in women with extremely dense breasts recommendations of the European Society of Breast Imaging (EUSOBI). European Radiology. January 2022.
11. Berg et al. Ultrasound as the Primary Screening Test for Breast Cancer: Analysis From ACRIN 6666. JNCI J Natl Cancer Inst (2016) 108(4): djv367
12. Yang L et al. Performance of ultrasonography screening for breast cancer: a systematic review and meta-analysis. BMC Cancer (2020) 20:499. https://doi.org/10.1186/s12885-020-06992
13. Busch et al. Association of State Dense Breast Notification Laws with supplemental Testing and Cancer Detection after Screening Mammography. American Journal of Public Health. 2019;109:762–767. doi:10.2105
14. Jia M et al. Diagnostic performance of automated breast ultrasound and handheld ultrasound in women with dense breasts. Breast Cancer Research and Treatment (2020) 181:589–597
15. Butler et al. Screening Breast Ultrasound: Update after 10 years of Density Notification laws. American Roentgen Ray Society. 2020; 214:1424–1435
16. Okello et al. Breast cancer detection using sonography in women with mammographically dense breasts. BMC Medical Imaging.2014.